Order of Reading a Chest X Ray
Purpose [edit | edit source]
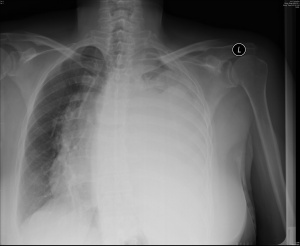
Chest X-rays is a painless, non-invasive test and is the most normally preferred diagnostic exam to produce images of center, lungs, airways, blood vessels and the bones of the spine and breast[i] [2].
Technique [edit | edit source]
An X-ray uses electromagnetic waves and ionizing radiation to create pictures of the inside of your body.
The procedures involves positioning the body between the machine that produces the X-rays and a plate that that creates the image digitally or with X-ray motion-picture show[1].
- To obtain the forepart view:
- Posterior - Inductive (PA). This is the well-nigh common and preferred type of chest Ten-Ray. Posterior - anterior refers to the direction of the Ten-Ray beam travel.; i e. X-Ray beams hit the posterior part of the chest before the anterior part. To obtain the image, the patient is asked to stand with their chest confronting the film, to agree their arms upwardly or to the sides and curlicue their shoulders forward. The X-ray technician may then ask the patient to have few deep breaths and agree it for a couple of seconds. This techniques of holding the breath generally helps to get a clear film of the eye and lungs on the image.

- Inductive - posterior (AP): This type of chest X-Ray is generally less preferred considering the image of the center and mediastinum is less clear and focused in this projection. To obtain AP image, the patient is asked to stand up with their dorsum against the flick. If the patient is unable to stand, an AP image tin also exist taken with the patient sitting or supine on the bed.
- Decubitus: This type of X-Ray shows a frontal view of the breast when the patient is lying on their side(south). Decubitus X-Ray can exist performed to assess the air inside the lung, the presence of free fluid, or airway obstruction.
- Posterior - Inductive (PA). This is the well-nigh common and preferred type of chest Ten-Ray. Posterior - anterior refers to the direction of the Ten-Ray beam travel.; i e. X-Ray beams hit the posterior part of the chest before the anterior part. To obtain the image, the patient is asked to stand with their chest confronting the film, to agree their arms upwardly or to the sides and curlicue their shoulders forward. The X-ray technician may then ask the patient to have few deep breaths and agree it for a couple of seconds. This techniques of holding the breath generally helps to get a clear film of the eye and lungs on the image.
two. To obtain the side-view (lateral): A lateral image is commonly taken to complement the frontal view. A lateral prototype is useful to localise a lesion since, together with a frontal paradigm, it allows a iii-dimensional analysis. To obtain a lateral image, the patient is asked to turn and place i shoulder on the plate and heighten their hands over their caput. The technician may again ask the patient to take a deep breath and concord it.

The post-obit videos explain the differences between the above types of chest X-Ray:
Analysis [edit | edit source]
Basic Checks[3] [edit | edit source]
Reading the breast 10-ray systematically reduces the take a chance of missed diagnosis. There is no ane recommended analysis methodology; some may choose to read a chest Ten-Ray in an anatomical club and some may cull to use a mnemonic. Nonetheless, everyone should begin analysing an X-Ray by checking the following details:
- Patient'southward full proper name and engagement of birth
- Appointment and time of the X-Ray taken. There could be a few images taken on the same solar day.
- Image Notation
- Correct (R) or Left (left side)
- Image projection: PA (posterior-anterior) or AP (anterior-posterior) or lateral
- Patient's position. Check whether the patient is upright, semi-erect, or supine when the image was taken.
- Paradigm Quality (R.I.P)
- R - Rotation. Check whether the patient's position is rotated. The patient is Not rotated if the spinous processes are equidistant from the medial ends of the clavicles.
- I - Inspiration. Bank check whether the 5 - 7 inductive ribs intersect the diaphragm in the mid-clavicular line. If the intersection happens in inductive ribs 8 or more, and so the lungs are hyperinflated.
- P - Penetration. Bank check whether the spine and the spaces between the ribs tin can be seen through the eye; which indicates that the X-ray exposure is adequate.
- Is at that place any previous films for comparing purposes?
- Foreign objects such equally lines, tubes, pacemaker, drains, etc. Foreign objects tin too exist non-medical such equally bullets, glass, etc.
- Wait at the big picture. You may want to starting time looking at the chest ten-ray from a distance and then motility closer. This will allow you to look at the big moving-picture show and encounter major abnormalities (if any).
Systematic Assessment[3] [4] [edit | edit source]
The near commonly used mnemonic arroyo to assess the details of Chest X-Ray is the following:
| Mnemonic | Explanation | Note |
|---|---|---|
| A | Airways | The trachea should be central or slightly to the right. If information technology is deviated, check whether it is due to the patient's position or another pathological crusade. |
| B | Basic and soft tissues | Assess the bones visible in the paradigm from top to bottom. The edges of the bones should be smoothen, otherwise a fracture may be indicated. As well assess for bone density, oedema or metastatic lesion. |
| C | Cardiac | On a PA prototype, the centre'due south width should exist less than 50% of the chest width. On an AP image, information technology should be between 50-lx% of the breast width. |
| D | Diaphragm | The right diaphragm is ordinarily college than the left. The costophrenic and cardiophrenic angles should be clearly visible. The blunting of those angles may signal effusion. |
| Eastward | Edges of the Heart | The edges of the heart should exist clearly defined. Otherwise, there may be consolidation in the side by side lung lobes. |
| F | Fields and Fissure | Check for whatever absence of normal lung markings in both fields. Besides check for opaque masses, consolidation, or fluid. |
| G | Great Vessels or Gastric bubbles | Assess the aorta and pulmonary vessels. The aortic knob should be visible. A normal gastric bubble can exist seen below the left diaphragm. |
| H | Hila | The left hilum is commonly higher than the right. Visible lymph nodes around the hila are an abnormal finding. Also cheque for masses or calcification around the hila. |
The post-obit video explains how to analyse a Chest- x-ray in nutshell:
Detecting Pathology [edit | edit source]
Atelectasis= Plummet, alveloi filled with fluid or collapse. Mutual postal service-surgery.
| Airways (Trachea) | Breathing (Lung fileds) | Cardiac | Diaphram | |
|---|---|---|---|---|
| Retained sputum | Consolidation = White. Follow contours of a lobe. No midline shift | |||
| Lung volume | Mass occupied lesion = shifted away Collapse = Shifted towards | Hyperinflation= Dark lung fields, blunting of costophrenic angles. No midline shift. Flat ribs Atelectasis = Pull trachea towards, wihite in appearance | Left lower lobe plummet = Flattening of left border | Hyperinflation= Raised Collapse= Raised |
| V/Q mismatch | Consolidation = White. Follow contours of a lobe. No midline shift Pulmonary odema= White. Batwing opacities, septal lines and localised collapse and pleural effusion. | Enlarged- Covers > 50% of cardiothoracic space Hilar markings- Congestion, cardiac failure | ||
| Respiratory pump failure | Pneuomthorax = shifted away | Pluerual effustion= Meniscus sign, push button trachea away, white. | ||
Evidence [edit | edit source]
- A written report conducted past Tape and Mushlin (1988) to study the effect of routine chest x-rays of pre-operative patients at chance for postoperative disease. Patient records from 341 admissions were reviewed to determine the relationship between chest x-ray results and postoperative chest complications. Patients who had major abnormalities had a 40% postoperative complication rate, compared with ix% for those with normal x-rays; but just 13% of the complications occurred in patients with major abnormalities. Nine patients had x-ray findings that led to clinical action: three with potentially beneficial direction changes (congestive center failure in ii, fibrosis in 1) and half dozen with potentially detrimental clinical activeness (false diagnosis of tuberculosis in 2, false diagnosis of nodules in 2, falsely normal chest x-ray in 2). None of 50 surgical cancellations occurred every bit a result of an abnormal x-ray. All the beneficial effects owing to preoperative breast 10-rays accrued to patients who had clinical evidence of breast disease. The authors conclude that routine chest x-rays were not helpful in improving patient outcomes. They recommend ordering preoperative chest x-rays based on clinical indications so that the likelihood of false positives and false negatives and their associated detrimental effects can be minimized[5].
- Comparison with other imaging method[half-dozen]. Computed Tomography (CT) has been suggested equally the gold standard of chest imaging due to its high sensitivity and specificity, Withal, due to its high-cost, length of procedure, and difficulty to access, CT has non replaced Ten-Ray as the primary chest imaging tool. A more than novel diagnostic tool, Lung Ultrasound (LUS), has shown to exist more practical and cheaper than CT whilst being more precise than X-Ray in producing chest images. However, more than robust research needs to exist washed to evaluate LUS accuracy in various pathologies in order for a comparing with chest X-Ray to be accurately fabricated.
Resources [edit | edit source]
100 Normal Breast X-Rays
Radiology Masterclass
Introduction to Chest Radiology
References [edit | edit source]
- ↑ ane.0 1.1 RadiologyInfo.org. X-Ray (Radiography) - Chest.http://www.radiologyinfo.org/en/info.cfm?pg=chestrad
- ↑ National Heart, Lung, and Claret Found. Chest Ten-Ray. https://www.nhlbi.nih.gov/health/wellness-topics/topics/cxray
- ↑ 3.0 3.1 Radiology Masterclass. Chest 10-Ray Systematic Approach. https://www.radiologymasterclass.co.uk/tutorials/chest/chest_system/chest_system_start (accessed 19 March 2018)
- ↑ Duong M, Timoney P, MacNicholas R, Kitchen J, Mustapha Chiliad, Arunasalam U. ABC'south of Chest X-Rays. TSMJ 2001; 2: xi-xiv
- ↑ Tape TG, Mushlin AI. How useful are routine chest 10-rays of preoperative patients at risk for postoperative chest disease?.Journal of general internal medicine 1988; 3.ane: 15-20.
- ↑ Coxon J, Kilmurray SF, Stewart HC. Chest X-Ray and Lung Ultrasound: A literature review of the electric current primary imaging tool, does it provide best do? Journal of ACPRC 2017; 49: 36-50
navarretetere1988.blogspot.com
Source: https://www.physio-pedia.com/Chest_X-Rays
0 Response to "Order of Reading a Chest X Ray"
Post a Comment